Maintaining comprehensive medical records is important for delivering quality patient care and mitigating legal risks. Well-prepared and securely stored medical charts not only support the successful defense of legal actions but are also essential for attorneys to demonstrate various healthcare encounters and their outcomes. Patient records serve as crucial evidence in cases related to personal injury, medical malpractice, workers’ compensation, or product liability. Identifying missing records is a key part of the medical record review in such cases, and the collaboration between healthcare providers and legal professionals can be optimized through the services provided by medical review companies.
Lawyers handling health litigation face the challenge of identifying missing records. The assistance of trained professionals becomes essential in collecting comprehensive and relevant information, such as the names of healthcare providers, complaint details, dates of service, tests ordered, medications, treatment outcomes, and contact information.
MOS’ medical review services ensure thorough documentation for stronger litigation support!
Call us at (800) 670-2809!
Insufficient or Missing Medical Records
Insufficient or missing healthcare records refer to situations where the records pertaining to a patient’s healthcare encounters lack essential information or are incomplete. Missing records may include:
- Incomplete patient history – Missing details about the patient’s healthcare history, including pre-existing conditions, allergies, previous treatments, and surgeries.
- Incomplete examination records – Lack of thorough documentation regarding the physical examinations conducted by healthcare providers, which is essential for assessing the patient’s current health status.
- Unrecorded diagnostic tests – Failure to document the results of diagnostic tests, such as laboratory reports, imaging studies, or other medical tests, can lead to incomplete information for healthcare decision-making.
- Inadequate treatment documentation – Missing or insufficient information about prescribed medications, treatment plans, and therapeutic interventions may compromise the continuity and effectiveness of patient care.
- Unclear progress notes – Insufficient or unclear progress notes that detail the patient’s response to treatment, changes in condition, and ongoing care plans.
- Incomplete discharge summaries – Failure to provide a comprehensive summary of the patient’s hospital stay, including the reason for admission, treatments received, medications prescribed, and post-discharge care instructions.
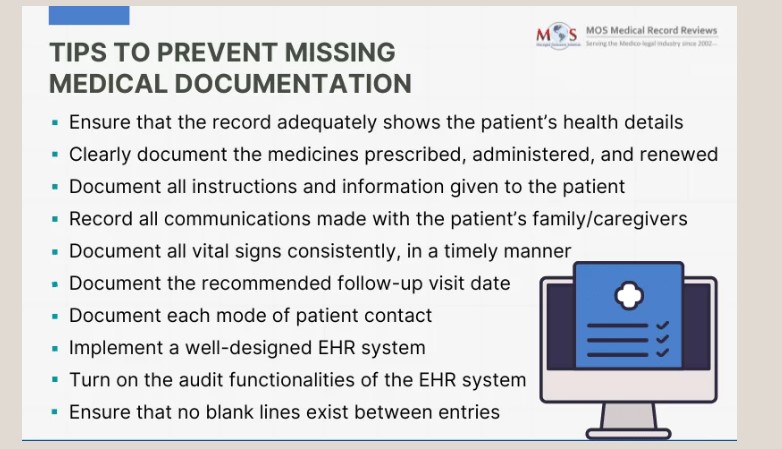
How to Prevent Missing Medical Documentation?
9 Key Strategies to Prevent Missing Medical Records
- Implement comprehensive documentation policies: Develop clear and comprehensive policies that outline the essential elements required in records. Ensure that all healthcare professionals are familiar with and adhere to these guidelines.
- Provide ongoing training: Conduct regular training sessions for healthcare staff on the importance of thorough documentation. Keep them updated on any changes in documentation requirements, coding standards, and legal regulations.
- Implement Electronic Health Records (EHR) systems: Invest in advanced EHR systems that prompt healthcare providers to enter the required information and generate alerts for missing data. Electronic systems can improve accuracy and completeness of records.
- Utilize checklists and templates: Provide healthcare professionals with standardized checklists and templates for various types of encounters, procedures, and examinations. This helps ensure that no critical information is overlooked.
- Encourage real-time documentation: Promote the practice of real-time documentation during patient encounters. This reduces the likelihood of forgetting details and minimizes the risk of incomplete records.
- Conduct regular audits: Implement routine internal audits to assess the completeness and accuracy of the medical documentation. This proactive approach helps identify any deficiencies and allows for corrective measures to be implemented promptly.
- Hire documentation specialists: Employ dedicated specialists or medical reviewers who are trained to review and ensure the completeness of healthcare records. Their expertise helps them spot missing information before it becomes a significant issue.
- Implement quality assurance protocols: Establish quality assurance protocols for medical documentation, including a review process to verify the completeness of records before finalizing and filing. This additional layer of scrutiny can detect any oversights.
- Stay informed about regulatory changes: Regularly update healthcare professionals on changes in regulations, coding standards, and documentation requirements. Staying informed helps ensure that the record management practices align with the latest industry standards and compliance expectations.
Listen to our podcast on –
How to Prevent Missing Medical Records
https://www.youtube.com/watch?v=uK5xAHoGIZM
Professional Medical Review Services Can Provide Chart Audits
Professional medical review services provide valuable assistance to healthcare providers and facilities by conducting thorough chart audits. These audits play a crucial role in evaluating the quality and accuracy of documentation. A comprehensive review encompasses the identification of missing details and ensures the inclusion of essential information in the medical chart.
This process involves scrutinizing the patient’s demographic details, pinpointing missing or incomplete records, specifying the hospital service provider from which the required information is to be retrieved, determining the date or period of the record, explaining why the specific record is necessary, and discerning whether the record is conclusively missing or potentially missing. This approach helps providers enhance the completeness and reliability of their healthcare records, contributing to improved patient care and legal preparedness.
Your solution to incomplete records is just a click away.
Contact us now at (800) 670-2809! for expert medical review services!