A clear review and summary of the medical chart and health information of patients, preferably by a litigation support team, provides the attorney important medical insights that are essential to develop the argument. While physicians need patients’ health record review to get a clear view of patient diagnosis, physical exam details and the treatments and medications given, and to check the current patient health, plaintiff and defense attorneys require medical chart review to strengthen the medico-legal cases they are dealing with.
Medical record review is a comprehensive process that involves reviewing key parts of a patient’s chart. This chart includes medical information, such as medical history, family history, developmental history, surgical history, and testing results. The review of medical records also involves analyzing charts including clinical data, physical exams, and orders for lab tests. Reviews help to determine the legality of the claim and the extent of injury or illness of the plaintiff.
Discover how our expert team can assist you in conducting thorough and accurate medical chart reviews.
Different types of chart reviews are available. Medical records are compiled, maintained, and reviewed for medical necessity determinations, personal injury cases, workers’ compensation claims, social security disability claims, medical research, and clinical documentation.
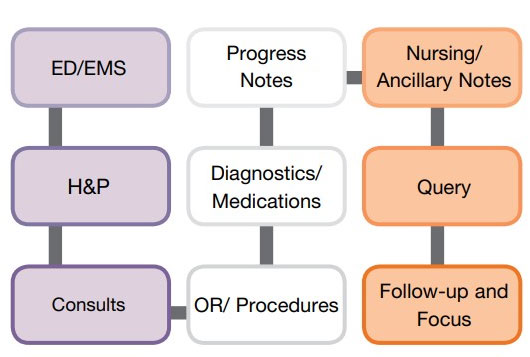
In their whitepaper, the Association of Clinical Documentation Integrity Specialists (ACDIS) has highlighted the process of conducting a medical record review.
Given below is an example of the chart review workflow given by ACDIS.
Watch the detailed video of the key parts that should be reviewed in a medical chart:
Key Areas to Review in a Medical Chart
In a medical record analysis, it is important to evaluate certain areas of the medical chart that contain key information about the treatment given to a particular patient. Experts.com has discussed such key areas in an article.
Major areas that are reviewed include:
Emergency Department (ED) Notes
Notes from emergency medical services (EMS)
- provide a baseline of medical necessity and clinical support
- capture relevant past medical history like appropriate chronic conditions
- highlight differential diagnoses that require clarification in the documentation
Physician’s Orders
Reviewing the physician’s orders helps to determine whether
- orders were carried out by the nurses or other appropriate staff
- orders were taken care of in a timely manner, and
- they are relevant to the patient’s diagnosis
Progress Notes
Progress notes prepared by physicians and nurses are crucial to
- create a timeline about the patient’s condition from admission to discharge
- get a perspective on physicians’ and nurses’ evaluation of the patient
Lab Reports
With lab test results, attorneys can
- collect evidence regarding the diagnosis of the patient
- even point out a condition that may be undiagnosed by the physician
History and Physical
Reviewing H&P helps to evaluate the physician’s work and
- ensure that the physician documented the clinical indicators which support the diagnoses
- determine that the treatment prescribed was appropriate
Medications
Medications reported in the medical record include
- medicine type provided, administration and dosage of the same
- comparison of medications given with the physician’s orders
As any medical record, including image films, is a key source of information in a medical related case, it is important to make sure that the review of electronic medical records as well as paper notes is done by experienced reviewers. Chart review is a critical component of the medical record review process as it provides insight into the patient’s condition and treatment options. Experienced medical record review companies collect, organize, review, and interpret medical records relevant to the case and maintained by healthcare facilities. They prepare a clear medical chronology and summary that attorneys need to develop and argue their case successfully.
Looking for cost savings? We offer 30 – 40% cost savings without compromising quality and accuracy.