AI Medical Claims Review to Save Time, Improve Accuracy, and Maximize Value
Streamline Claims Review with AI-powered Intelligence
Processing and reviewing medical claims for litigation or insurance can be time-intensive, error-prone, and expensive. Our advanced AI medical claims review platform streamlines the process using cutting-edge AI technologies—automating the extraction, validation, and summarization of clinical and billing data from large medical records.
Whether you’re preparing for a deposition, contesting a claim, or verifying costs, our solution delivers fast, accurate, and audit-ready results—all while reducing physical effort and review timelines.
Our services are designed for:
- Attorneys and legal teams involved in insurance litigation, personal injury, medical malpractice, and mass tort cases.
- Health plan insurers and TPAs (third party administrators) seeking accurate and expedited medical claims validation.
- Physicians and medical experts supporting claims assessments, IMEs.
ReviewGenX: AI-powered Medical Bill Review
Our medical record review is powered by ReviewGenX, based on DeepKnit AI, that utilizes advanced Natural Language Processing (NLP), Intelligent Character Recognition (ICR), and rules-based auditing to analyze, verify, and dispute medical bills with unmatched accuracy. Developed on proprietary Large Language Models (LLMs) and trained using real-world clinical data, it produces evidence-backed, dispute-ready evaluations at a speed and precision impossible with manual review.
Designed for effortless adoption, ReviewGenX integrates seamlessly with:
- Major EHR platforms including Cerner, Epic, and Allscripts
- HL7/FHIR-based healthcare data systems
- Claims and case management applications
- Legal technology platforms such as Everlaw and Relativity
The result is a streamlined workflow, centralized documentation, and stronger support for both insurance and legal teams.
How Our AI Medical Claims Review Works
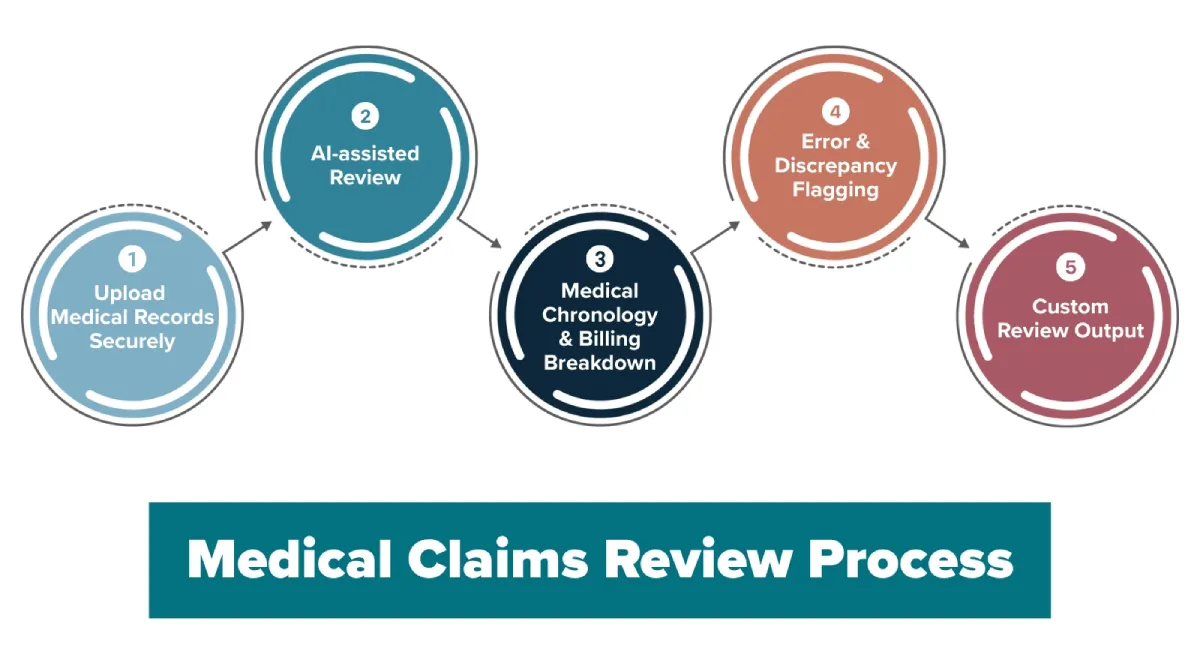
Upload Medical Records Securely
Upload your scanned or digital medical records via our encrypted portal.
AI-assisted Review
Medical Chronology & Billing Breakdown
Error & Discrepancy Flagging
Custom Review Output
What Sets Our AI Claims Review Solutions Apart
- Automated Data Extraction from Medical Records
Our AI tool reads and extracts diagnoses, procedures, provider notes, and timelines from structured and unstructured data—including scanned PDFs. - Billing & Coding Accuracy Checks
We identify incorrect CPT/ICD codes, undocumented procedures, and upcoding/downcoding patterns—important for legal defences or claim denials. - Comprehensive Chronology & Case Timeline
Our platform reconstructs medical events into a logical, structured chronology with associated billing codes and provider actions. - Error Flagging and Medical-Legal Insights
Automatically highlights inconsistencies, gaps in care, duplicate charges, and causality issues—empowering you with decision-ready insights. - Customizable Reports for Different Stakeholders
Choose output formats suited for attorneys, insurance adjusters, or IME consultants—customized summaries, red flags, and detailed breakdowns. - Fast Turnaround – Up to 70% Time Savings
Handle urgent claims and court deadlines with reviews completed in minutes, not days.
Security & Compliance You Can Rely on
HIPAA-compliant Platform
End-to-end Encryption
Audit Trails & Role-based Access Controls
Fully Documented Reports for Legal & Insurance Review
Frequently Asked Questions
Can your system handle scanned handwritten records?
What formats do you support for input and output?
Do you offer hybrid AI + human review options?
Can we integrate this into our case or claims management system?
Built to Scale with Your Legal and Insurance Workflows
Get Started – See the Power of AI in Action
Related Posts
Five Ways AI Reduces Errors in MSA Documentation
What if a single missed line in a medical record could delay a settlement by months, or worse, trigger a costly CMS rejection? For attorneys, insurers, and claims professionals managing Medicare Set-Asides (MSAs), this isn’t a hypothetical risk. It’s a tussle they...
AI for Medicare Set-Asides: Redefining Medical Record Review
Did you know that a whopping 750,000+ Medicare beneficiaries are involved in workers’ compensation cases annually, and each claim requires meticulous medical record review before a Medicare Set-Aside (MSA) can be approved? Now imagine reviewing all of that manually;...
Why AI-powered Medical Record Review is a Game Changer for Personal Injury Cases
Personal injury litigation depends on a meticulous, defensible reading of sometimes thousands of pages of medical records. Medical records tell the story of the injury, its cause, its consequences and also help estimate the value of the case. AI-powered medical record...



