The way healthcare documentation is created, stored, and accessed in the country has undergone a significant transformation over the past decade. Computerized medical documentation, primarily in the form of EMRs and EHRs, has reshaped how attorneys interact with patient records. Paper medical charts, once considered the gold standard in hospitals and private practices, have largely given way to electronic medical records (EMRs) and electronic health records (EHRs). This shift was accelerated by the Health Information Technology for Economic and Clinical Health (HITECH) Act, Medicare and Medicaid incentives, and more recently, by the COVID-19 pandemic, which drove a surge in telehealth and cloud-based documentation.
For attorneys, especially those involved in medical malpractice litigation, personal injury cases, insurance claims, or healthcare compliance, electronic medical records in litigation has become both a blessing and a challenge. On the one hand, attorneys now have access to clearer, more standardized, and often more comprehensive records than ever before. On the other hand, new complexities have emerged around authenticity, privacy, EMR metadata for attorneys, and the interpretation of templated or auto-generated content.
As of now, EMRs are no longer just repositories of patient information; they are capable of accommodating AI tools, driving clinical decision support and interoperability functions that connect hospitals, labs, pharmacies, and insurers. Understanding how these systems work, and where they fall short is vital for attorneys.
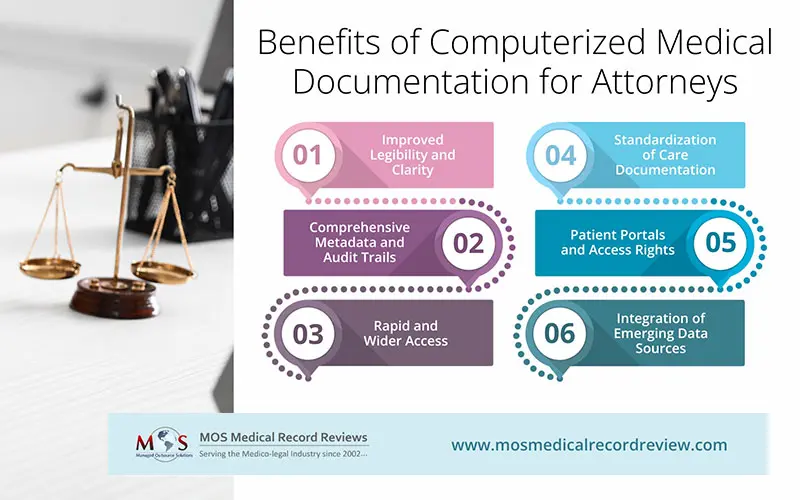
What Are the Benefits of Computerized Medical Documentation for Attorneys?
- Improved Legibility and Clarity
EMRs offer typed, standardized entries with built-in prompts. Each note is time-stamped and attributed to a specific provider, eliminating any confusion about who made an entry and when.
- Comprehensive Metadata and Audit Trails
Modern EMRs include comprehensive audit trails that track every login, entry, update, and deletion. For attorneys, this means a transparent chain of custody: who accessed the record, what updates were made, and whether documentation was altered retroactively. Data of this magnitude can be invaluable in both malpractice defense and plaintiff cases.
- Rapid and Wider Access
With most major health systems now using interoperable, cloud-based platforms (built on HL7 FHIR standards), attorneys can gain access to more complete patient records faster than they did with paper charts. Records from hospitals, labs, imaging centers, and even pharmacies can be compiled with more efficiency. This accelerates case preparation and discovery.
- Standardization of Care Documentation
EMRs are designed to align with U.S. healthcare standards of care. Built-in prompts for allergies, medication reconciliation, consent forms, and safety checks reduce the risk of omissions. For defense attorneys, this often demonstrates that providers met basic documentation requirements, and for plaintiff attorneys, failure on the part of providers to complete the required fields can strengthen claims of negligence.
- Patient Portals and Access Rights
The federal 21st Century Cures Act requires healthcare providers to grant patients electronic access to their medical records. Attorneys can make use of this patient access to obtain relevant records directly from clients, often faster than the formal, traditional medical record requests.
- Integration of Emerging Data Sources
Wearable devices, telehealth visits, and remote monitoring tools have the capability to feed data directly into EMRs. Attorneys may be able to use continuous heart rate, glucose levels, or physical activity data to substantiate claims or defenses in ways that weren’t possible even five years ago.
Challenges of Computerized Medical Documentation for Attorneys
- Copy-Paste and Templated Entries
One of the biggest problems with EMRs is “note bloat”, which simply means lengthy records that are filled with copied text, repeated templates, and irrelevant details. Attorneys may find multiple visits with identical wording, making it difficult to distinguish genuine clinical observations from boilerplate. This can obscure important facts or lead to disputes over whether a provider truly exercised judgment.
- Data Integrity and Authenticity Questions
While audit trails provide transparency, attorneys must still address whether EMRs can be manipulated. Retroactive edits, “late entries,” and auto-corrections can raise suspicions. In litigation, demonstrating that records are authentic and unaltered requires careful handling of native formats, metadata, and compliance with the Federal Rules of Evidence on electronic documents.
- Interoperability Gaps
Despite major advancements in technology, interoperability across all U.S. healthcare systems remains imperfect. Smaller clinics may still rely on outdated systems, and scanned documents or faxed records are sometimes uploaded without searchable text. Attorneys must be vigilant about missing lab records, imaging, or outside consultation notes that could significantly alter the scope of a case.
- Privacy and Cybersecurity Risks
Data breaches still remain a major cause of concern. With advancing technology to safeguard data, cybercriminals are parallelly rising to the challenge, with even encrypted EMR databases being their targets. For attorneys, HIPAA compliance and patient privacy rights must be carefully balanced during discovery. Mishandling of electronic records could not only lead to case setbacks but also attract regulatory penalties.
- Narrative Limitations
Although EMRs allow narrative notes, providers often rely on structured fields and drop-down menus to save time. As a result, the nuance of a patient’s condition may be under-documented. For attorneys, this lack of narrative context can make it harder to accurately establish liability, intent, or the provider’s clinical reasoning.
- Costs and Access Delays
Even with patient portals, obtaining full, certified EMR records can be costly and time-consuming. Hospitals may charge retrieval fees, and producing native electronic formats with metadata often requires back-and-forth negotiation. In large cases, reviewing voluminous EMRs can itself become a resource-intensive task.
Best Practices for U.S. Attorneys Handling EMRs
- Request Native Formats: Ask for EMRs in their original electronic form, including audit logs, rather than just PDFs or printed versions.
- Scrutinize Metadata: Use forensic experts wherever necessary to analyze timestamps, edits, and authorship.
- Be Alert to Templates: Compare multiple visits for copy-paste language to challenge the accuracy of documentation.
- Check for Missing Pieces: Confirm whether external labs, radiology images, or telehealth notes were promptly integrated into the record.
- Protect Privacy: Make sure all record requests and disclosures comply with HIPAA and state privacy laws to avoid any liability.
- Use Experts: Collaborate with medical and IT experts who have the expertise to handle EMR systems.
Final Thoughts
Computerized medical documentation in the U.S. has matured into a powerful tool for healthcare and litigation alike. For attorneys, the benefits of clear records, robust audit trails, faster access, and standardized care documentation are significant. However, medical documentation challenges like authenticity disputes, templated content, privacy risks, and narrative gaps are equally important to manage.
In this context, medical record analysis plays a crucial role—helping legal teams identify inconsistencies, uncover missing details, and validate information in ways that raw electronic medical records often cannot.
In 2025, attorneys who understand how EMRs work, what pitfalls to anticipate, and how to leverage metadata and audit trails will be best equipped to use electronic medical documentation effectively in medical malpractice, personal injury, and healthcare litigation. The key lies in balancing the efficiency of digital records with a critical eye for accuracy and authenticity.