A workers’ compensation case is evaluated on the basis of the documentation of the injury or illness in the claimant’s medical records. The medical chart reveals the extent of the injury or severity of the illness and informs a request for treatment. Since these records are legal evidence, they are reviewed to determine the legitimacy of a case and medical record review for attorneys is an important service in this regard. Workers’ compensation attorneys use the service provided by a medical record review company, wherein the review is done by medical and paramedical professionals well-versed in the review process.
Gain the legal edge with comprehensive medical record reviews.
Essential Aspects Regarding Medical Records in Workers’ Compensation Claims
Now, let us discuss some important points to note about medical records in workers’ compensation.
- HIPAA and the workers’ compensation laws in individual states regulate the way in which sensitive medical information is disclosed and transmitted. HIPAA also determines how medical records are stored electronically and physically. HIPAA allows medical care providers to provide the required medical information of a person to his/her employer, state workers’ compensation administrators, and workers’ compensation insurance companies. The medical records disclosure act of each state clearly defines the information an employer is allowed to request.
- The medical details about the workplace injury must be collected and maintained on a completely separate form. Such records must be maintained in a separate file along with any other information that needs to be maintained in a confidential manner.
- There are restrictions as regards what information can be disclosed. A medical provider can disclose only the information that is required to pay for or treat an injured/ill worker. This means that the employer or workers’ comp personnel cannot gain access to the complete medical chart of a worker.
- Typically, employees may have to provide a medical authorization for release of the relevant medical records, if the insurance company makes such a request. Employees should not sign a blank release form because they are required to release only those records related to the treatment of their injury or illness. The authorization form should contain the name of the medical provider to which the employee is signing a release of information. Ideally, a separate release of information can be made for each provider.
- Medical records are important legal evidence. To ensure fair claims processing, all records relevant to the claim will be considered.
- The obligation to pay for the medical records ordered falls on the defendant.
- Medical records that are inadequate could be used to deny even legitimate claims. Some of the reasons for claim denial are:
- The injury was not immediately reported
- Discrepancies are seen between the worker’s accident report and initial medical records
- The worker’s medical records show the presence of illegal drugs in his/her system
- The employee refused to give a recorded statement to the insurance company or sign medical authorizations.
- Medical records help in determining the medical necessity of a particular procedure or treatment provided to the employee.
- Medical records provide information regarding any pre-existing health conditions. In most US states, workers’ compensation insurance covers only the aggravation of an employee’s physical condition caused by the work-related injury or illness, not those caused by pre-existing conditions. If the employee’s pre-existing condition is medically related to their workers’ compensation claim, the benefits are likely to be affected.
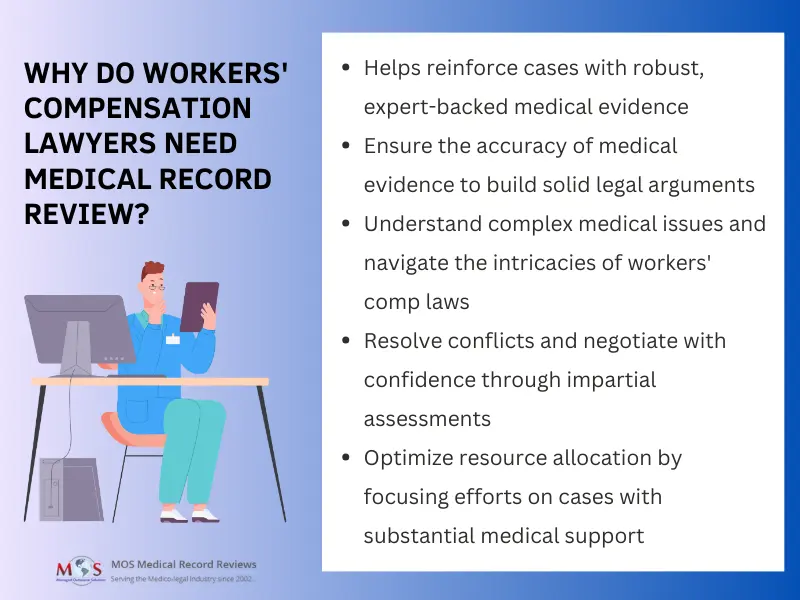
How Does Medical Record Review Benefit Workers’ Compensation Lawyers?
Proper review of medical records offer several advantages to lawyers involved in workers’ compensation cases:
- Evidence evaluation: Lawyers can use accurate review of medical records to obtain the medical evidence needed to support their clients’ claims. These reviews provide objective and expert opinions on the medical evidence, which can strengthen the case and increase the chances of a favorable outcome.
- Objective assessment: Independent medical experts conducting the reviews offer unbiased and objective assessments of the medical records. This objectivity can carry substantial weight in legal proceedings.
- Clarifying medical complexity: Workers’ compensation cases often involve complex medical issues. Medical record reviews can help lawyers understand the medical aspects of a case, enabling them to better advocate for their clients.
- Resolving disputes: In cases where there is disagreement between parties regarding the medical evidence, a well-conducted record review can help resolve disputes and lead to more expedited settlements.
- Effective communication: Lawyers can use the findings of medical record reviews to communicate effectively with the opposing party, insurers, and medical professionals. It can facilitate negotiations and lead to more favorable settlements.
- Reducing legal liability: Properly conducted medical record reviews ensure that the legal team is well-informed and acting within the bounds of the law, reducing the risk of legal liability related to workers’ compensation cases.
- Cost-efficiency:Accurate review can help lawyers identify cases with strong medical evidence, potentially saving time and resources by focusing efforts on cases with a
higher likelihood of success. - Educational resource: Lawyers can use medical record reviews as an educational resource to understand the medical aspects of workers’ compensation laws, ultimately enhancing their expertise in this area of practice.
Hope you are clear with the role of medical records in Workers’ Compensation claims.
Review of medical records are valuable tools for lawyers in workers’ compensation cases, providing them with expert analysis, objective assessments, and evidence support that can lead to better outcomes for their clients and more effective advocacy in the legal process. Professional companies providing medical review services and related solutions can make the entire claims processing efficient and uncomplicated.
Save time and resources with our efficient medical record review services.